This is less about neurology and sleep medicine, and more about all people who become patients.
I do find that particularly in the fields of neurology and sleep medicine, medications used to treat conditions in either specialty can be very potent or can interact with other medications, or have steep side effects in and of themselves.
I would like to give my recommendations about why and how a medication list should be kept.
And kept close by.
Why it should be kept:
-Mixing certain medications can cause multiple problems, such as nausea/vomiting, cardiac arrhythmias or worsen dizziness acutely to cause a fall and fracture, or can lower seizure threshold, etc. YOU WANT ME TO KNOW EVERYTHING YOU ARE ON WITHOUT CHANCE OF CLERICAL ERROR OR OTHERWISE, FOR THAT REASON ALONE.
2. It can help your doctor/doctors determine what medication may be causing which side effect you are experiencing versus just symptoms themselves.
-The timing of when a medication was started/stopped/raised/lowered is very important. It is not uncommon that I see patients with medications started, only to treat side effects of other medications because the timing couldn't be clarified.
-For example: I saw a pleasant older woman last week complaining of terrible nightmares and nausea. She was placed sometime ago on Aricept (donepezil). She was then placed on phenergan (as needed) for this nausea, and a low dose of trazodone to help her sleep through the nightmares.... She started developing leg "cramps" (difficult-to-describe muscle pains actually) for which a little magnesium oxide supplement was added, and headache/head "heaviness" for which naproxen (generic for Aleve) was added, which itself caused more stomach discomfort...So let's disentangle this: The patient has very mild cognitive impairment and was placed on donepezil for memory. She took it at night without food, and had only been taking it for a few weeks when her side effects of nightmares and nausea started (donepezil can cause nightmares if taken before bed and nausea if taken on an empty stomach). The phenergan for nausea didn't cause any problems, but trazodone for sleep caused muscle pain and headaches (both known potential side effects) and this stimulated two more medications, the magnesium and Aleve, the Aleve now causing more nausea by a different mechanism than donepezil....
Now, I'm not saying poly-pharmacy is inherently bad by any means. Multiple medical problems need to be treated with multiple medications. A person with memory problems can still have high blood pressure and heartburn and prostate enlargement and infections etc... If you thought I was telling you to throw away medications because more is always wrong, you read this erroneously.
I'm saying we should always be looking to simplify when possible. I'm saying YOU can help prevent poly-pharmacy instead putting all the detective work on your doctor/doctors; we should be the best stewards of our own health. IF the primary care doctor knew that donepezil had just been started by the neurologist, and taken at night, without food, then the simple trick could have been to just call the neurologist and ask them to fix the side effects they created or (if the primary care doctor already knew) have the patient take the donepezil in the morning or lunch with their food. Done. No phenergan/trazodone/magnesium oxide/naproxen needed. But the primary care doctor's ability to notice side effects caused by something the neurologist did is improved by a sharp-eyed and well-prepared patient, especially in today's insurance-dominated health care system which pushes doctor-patient encounter time limits to their thinnest possible.
3. It will diminish the likelihood of medication-medication interaction
Not just side effects... Some medication nullify the effect of others or can make other medications rise to toxic levels. For example, some medications for headache or epilepsy can decrease the effectiveness of birth control. Or medications can push epilepsy medications to poisonous levels or to low levels that will not stop seizures. Or I have patients on coumadin for cardiac & stroke concerns. Seeing that on their list reminds me to tell them to watch out for leafy green vegetables that can decrease the effectiveness of coumadin if taken in excess or to watch out for glucosamine (for joint health) because it can make coumadin work too well (bleed risk). But that's just the tip of the iceberg. I could write a series of blogs just about interactions between neurology medications and common over the counter medications or medications for common ailments
4. It will make your time with your doctor more efficient.
-Instead of the doctor facing away from you, looking at their computer and wading through a slight dishevelment of pixelated medication records, they can face you with your list and quickly address medication changes and updates going forward.
5. You may learn something you didn't known about your medications.
-When the patient shows me a list, I find myself telling them interesting facts about their medications, either in the context of their own health, or some tidbit that they may find useful in the future. Or I'll notice they are on a generic form which might be better tolerated if brand name, and I can write a letter to their insurance company on their behalf to get it approved.
------------------------------------------------------------------------
Date list most recently updated:
The doctors I see are:
Current medications & dose & when taken:
Date each medication started written beside it:
(Medications not taking and why... or above medication crossed through and a margin scribble explanation)
Other over-the-counter medications or supplements: (like Aspirin or St. John's Wort or vitamins)
Allergies to medication, or just bad response (like penicillin causing a rash versus Plavix causing your gums to bleed)
Bonus points for noting WHY you are on each medication.
Bonus points for somewhere reminding us of your current medical illness and major surgeries (yes, we should know, but reminders only help us).
------------------------------------------------------------------------
Here are some samples from my patients that I thought were worth showing.
I have removed their names and other identifiers.
What I like is that the person did what worked for them, which works for me.
This first example is the basic model: A note card with allergies on one side and list of medications on the other. Easy to update. Not quite as informative as it could be (per my recommendations above).

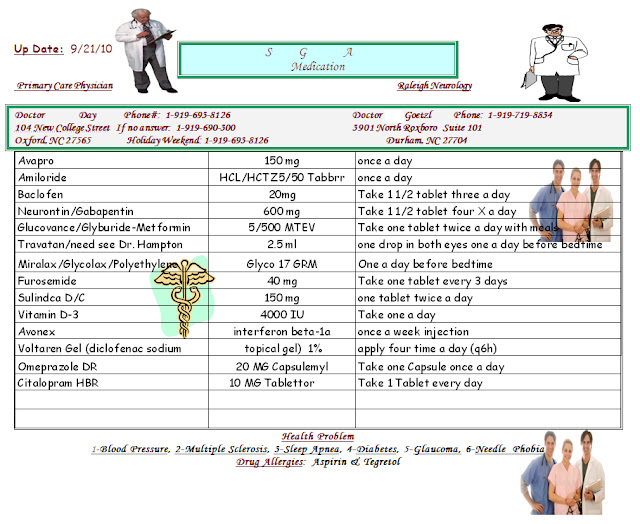
This next example is nice because I know exactly when they are taking each medication, the number to use to call their primary care physician right away if needed to discuss something. I quickly know their allergies, and some of their background medical issues I need to keep in the background of my thoughts as I treat this patient.
But... there are quite a few medications here; it'd be nice to know the patient knows why they are on these medications so they can help me get rid of some if not directly helpful. For instance, do they really need both Voltaren gel and Neurontin? Maybe the pain could be stopped by just one or the other.
This is a good one. I know who's prescribing what, why the patient believes they are on each medication, dose, timing, whether it's all the time or just when needed, allergies, and background medical diagnoses to consider. It's even recently updated.
This one is great in that it addresses a pet peeve of mine... and, yes, I will tell you in the office I am "peeved" that you have nooooo idea what medications you take, especially when you tell me it's "a little white pill." I can't argue with this patient about their pills; proof is at my fingertips. A lot of us have a hard time with crazy medication names like hydofluoroxyalbutereneflexozicamp... but most of us can remember a pill's shape, size, or unfortunate flavor.
It's often helpful for physicians to know if it's scored or not too.
If I had my way, I would combine this list and the one just above it.